How Sleep Affects Chronic Pain: The Missing Link to Healing
Introduction: Why Sleep and Pain Are a Vicious Cycle
If you’ve ever spent a night tossing and turning in pain, you know the cruel relationship between sleep and chronic pain. Poor sleep makes pain feel sharper, harder to tolerate, and more emotionally overwhelming. On the flip side, the very presence of pain often makes restful sleep impossible.
The result? A vicious cycle that feeds itself, leaving patients trapped in a loop of fatigue, flare-ups, and frustration. The good news: with the right science-backed strategies, you can break this cycle. In this article, we’ll explore how sleep affects chronic pain, why poor rest makes pain worse, and proven methods to improve both.
The Science of Sleep and Pain
How Poor Sleep Amplifies Pain Sensitivity
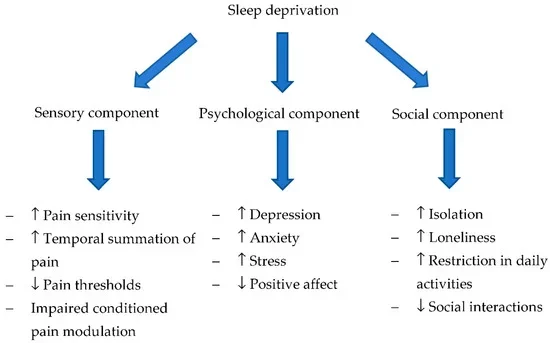
Research shows that just one night of poor sleep can heighten pain sensitivity by 20–40%. Lack of sleep reduces your brain’s ability to regulate pain signals, leaving your nervous system on “high alert.” Think of sleep as your body’s built-in reset button — without it, pain signals are amplified, and your threshold for discomfort plummets.
Brain Studies on Sleep Deprivation and Pain Thresholds
Functional MRI studies reveal that people with chronic insomnia show increased activation in brain regions tied to pain perception. Meanwhile, areas responsible for pain regulation (like the prefrontal cortex) go “offline” when sleep-deprived. Simply put: less sleep = more pain.
Why Pain Disrupts Sleep
Nighttime Flare-Ups and Nervous System Activation
Pain isn’t just physical — it’s neurological. Chronic pain often keeps the sympathetic nervous system (fight-or-flight mode) switched on at night, preventing the body from entering deep, restorative sleep. Patients describe this as a cycle of “wired and tired” — exhausted, yet unable to relax.
Anxiety About Sleep Worsens Insomnia
Many patients begin to dread bedtime. The fear of “another bad night” creates performance anxiety about sleep itself, leading to racing thoughts and stress. Ironically, this anxiety further disrupts the sleep cycle, deepening the connection between pain, stress, and poor sleep.
💡 Internal Link Opportunity: Direct readers to your “Breaking the Pain-Anxiety Cycle” blog post for deeper exploration of this relationship.
Evidence-Based Sleep Strategies for Pain Patients
Breaking the pain-sleep cycle requires practical, evidence-based solutions. Here are proven methods:
Keep a Consistent Sleep Schedule
– Go to bed and wake up at the same time every day (including weekends).
– Helps reset your circadian rhythm and stabilize hormone release.Optimize Your Bedroom Environment
– Keep the room cool (60–67°F).
– Block out noise/light with blackout curtains or a white noise machine.
– Invest in supportive mattresses and pillows for your specific pain condition.Practice Relaxation Techniques Before Bed
– Guided imagery, progressive muscle relaxation, or deep breathing.
– Consider mindfulness meditation, which has strong evidence for both pain and insomnia relief.
If pain keeps you up at night, schedule a consultation today. We’ll help design a personalized sleep + pain relief plan.
How Brain Retraining Improves Sleep
The Role of Pain Reprocessing Therapy (PRT)
PRT, a science-backed approach that retrains the brain to interpret pain signals differently, also improves sleep. When patients reduce fear and hypervigilance about pain, the nervous system relaxes—allowing restorative rest.
Calming the Fight-or-Flight Response
Techniques like PRT and mindfulness work by signaling safety to the brain. This reduces nighttime overactivation, helping patients transition into deep sleep cycles more smoothly.
💡 Internal Link Opportunity: Link back to your blog post on “Top Evidence-Based Pain Reprocessing Methods”for readers who want to explore PRT in detail.
Movement & Daytime Habits for Better Sleep
Exercise Timing and Its Impact
Exercise is a natural pain reliever and sleep promoter. But timing matters:
Morning or early afternoon movement supports circadian rhythms.
Avoid vigorous exercise within 2–3 hours of bedtime.
Limiting Caffeine and Using Light Exposure Wisely
Restrict caffeine after 2 pm.
Get natural sunlight in the morning to reinforce sleep-wake cycles.
Use dim light in the evening to signal the brain it’s time to wind down.
We’ll design a pain + sleep plan tailored to you. Book your consultation now and start restoring restful nights.
Case Story: Restoring Sleep to Restore Life
One patient, Sarah, lived with fibromyalgia and hadn’t slept more than 3 hours a night in years. By implementing structured sleep hygiene, reducing bedtime anxiety through PRT, and adopting a gentle morning exercise routine, she cut her pain in half and finally returned to consistent 7-hour sleep cycles.
Stories like Sarah’s prove that improving sleep isn’t just about feeling rested — it’s about reclaiming your life from chronic pain.
Conclusion: Unlock Healing Through Sleep
Without quality sleep, chronic pain recovery stalls. But when you restore rest, you unlock the body’s most powerful healer. By combining sleep strategies with brain retraining and lifestyle adjustments, patients can finally break free from the cycle of sleepless nights and painful days.